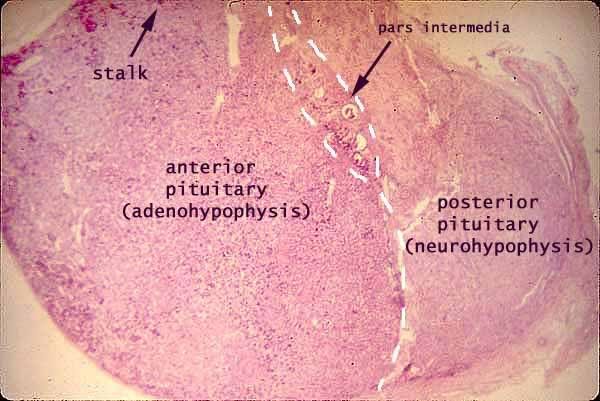
1. The anterior pituitary, also called the adenohypophysis.
2. The posterior pituitary, also called the neurohypophysis.
Both parts are attached by the pituitary stalk (also called neural stalk/ infundibulum) to the median eminence at the base of the hypothalamus.
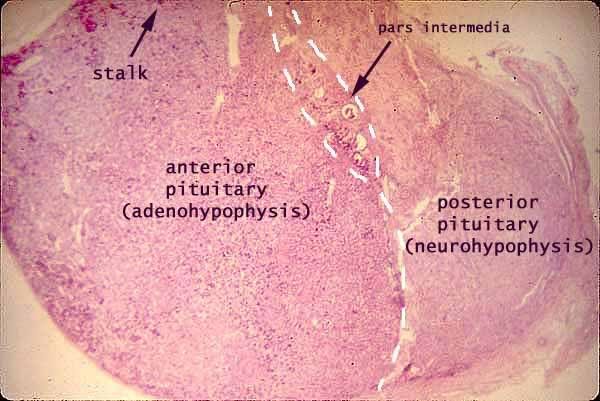
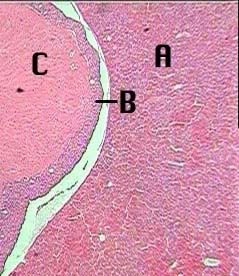
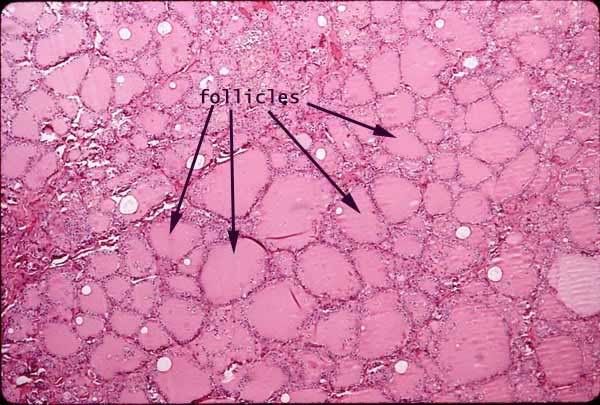
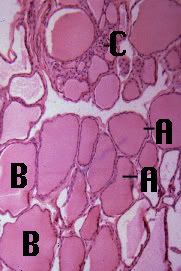
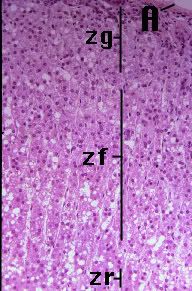
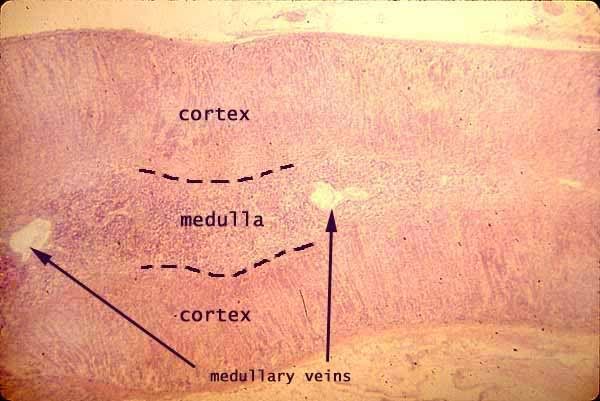
At 40x the pars distalis (A) and the pars intermedia (B) of the adenohypophysis (anterior pituitary) and the pars nervosa (C) of the neurohypophysis (posterior pituitary) can be observed. The pars tuberalis and infundibulum were not a part of this preparation. The pars distalis secretes Growth Hormone (GH), Thyroid-stimulating hormone (TSH), Adrenocorticotrophic hormone (ACTH), Follicle-stimulating hormone (FSH), Lutenizing hormone (LH),and Prolactin. The pars intermedia secretes Melanocyte-stimulating hormone (MSH). The pars nervosa stores ADH (antidiuretic hormone)and Oxytocin which were secreted by the hypothalamus.
Anterior Pituitary:
Terms to know and Recognize:
Pars Tuberalis
Pars Intermedia
Pars Distalis
Chromophobes- "color" phobes, don't stain well, nucleus appears in hollow hole
hypophyseal portal system
tropic hormones- hormone of anterior pituitary
MSH- melanocyte-stimulating hormone
Acidophils- secrete GH and PRL (Growth Hormone and Prolactin)
Basophils- secrete FSH, LH, ACTH, TSH (Follicle stimulating hormone FSH and leutinizing hormone LH are both referred to as gonadotrophs, adrenocoricotropic hormone ACTH, thyrotropic hormone TSH)
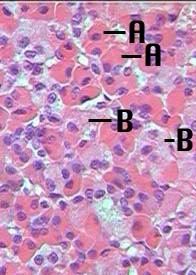
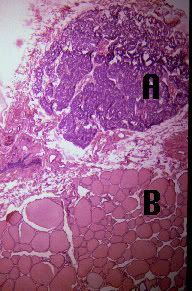
At higher magnifications the dark staining chromophils ( A) and the very light staining chromophobes (B) are easily distinguished.
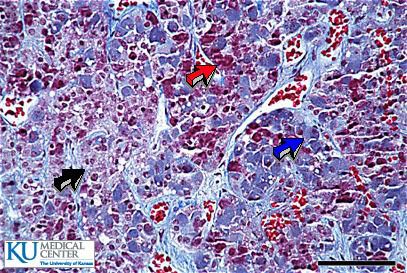
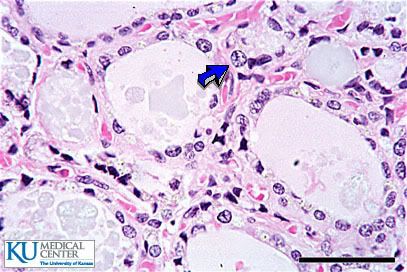
Chromophobes (black arrow), Eosinophiles (red arrow), Basophiles (blue arrow).
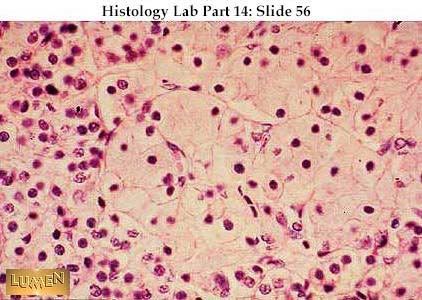
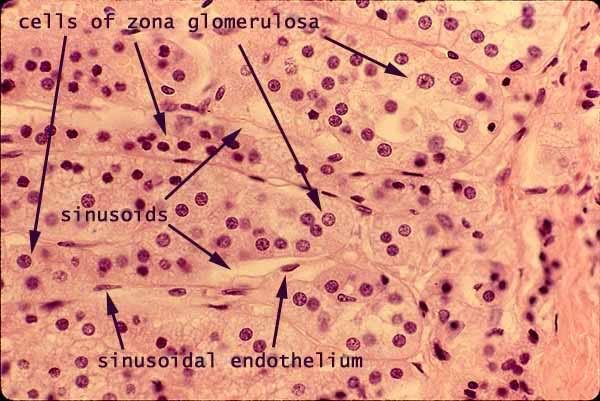
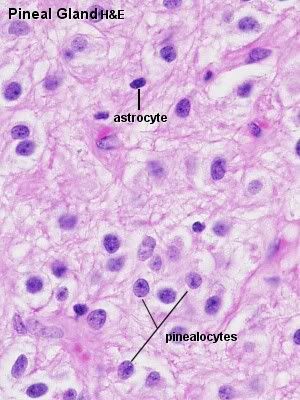
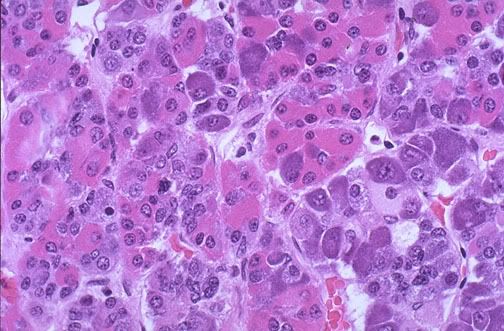 The normal microscopic appearance of the adenohypophysis is shown here. The adenohypophysis contains three major cell types: acidophils, basophils, and chromophobes. The staining is variable, and to properly identify specific hormone secretion, immunohistochemical staining is necessary. A simplistic classification is as follows:
The normal microscopic appearance of the adenohypophysis is shown here. The adenohypophysis contains three major cell types: acidophils, basophils, and chromophobes. The staining is variable, and to properly identify specific hormone secretion, immunohistochemical staining is necessary. A simplistic classification is as follows:The pink acidophils secrete growth hormone (GH) and prolactin (PRL)
The dark purple basophils secrete corticotrophin (ACTH), thyroid stimulating hormone (TSH), and gonadotrophins follicle stimulating hormone-luteinizing hormone (FSH and LH)
The pale staining chromophobes have few cytoplasmic granules, but may have secretory activity.
The Hypophyseal Portal system and Hormones explained simply
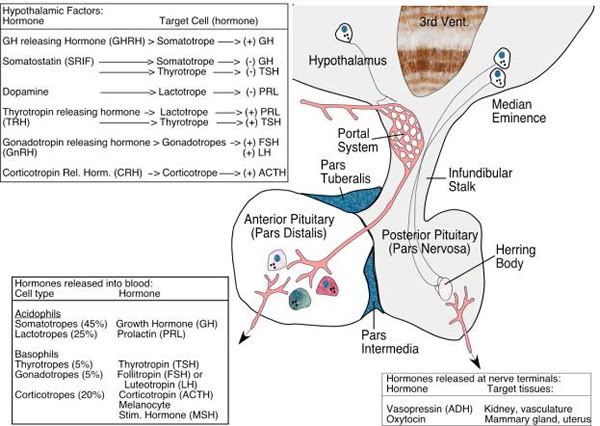
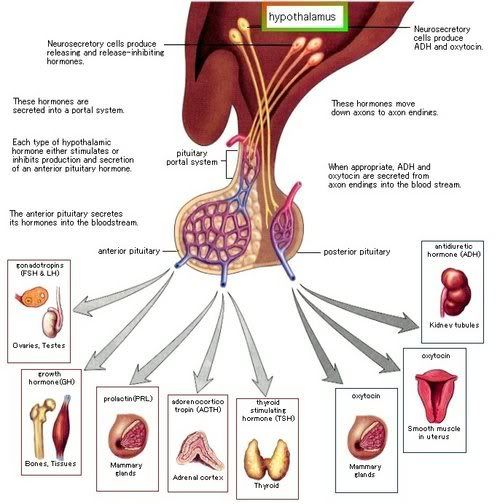
A portal system is a blood vessel circuit with 2 sets of capillaries instead of 1. The first capillary bed (1 capillary plexus) picks up the hypothalamic hormones from the ends of the axons. The second capillary bed (2 capillary plexus) drops off the hypothalamic hormones in the anterior pituitary. Connecting the 2 capillary beds are the hypophyseal portal veins.
Posterior Pituitary
Terms to Know:
Pars nervosa
Hypophyseal Tract- blood vessel portal with only one segment as in posterior pituitary
Pituicytes
Neural stalk- (aka) infundibulum
oxytocin
ADH- antidiuretic hormone
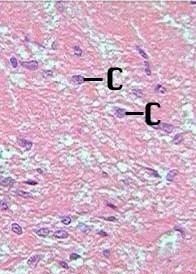
This region of the pituitary is non secretory. Its cells are neuroglial-like pituicytes (C).